Abstract
Background: Sickle Cell Disease (SCD) has established socioeconomic disadvantage resulting in increased healthcare utilization. Among the pediatric population, the implementation of preventative care measures within the medical home model has improved outcomes and lifespan. Area deprivation index (ADI) is an established method for quantifying socioeconomic disadvantage and has been shown to be associated with increased hospital readmission in adults and pediatric patients with chronic disease (Singh Am J Public Health. 2003, Kind et al. Ann Intern Med. 2014). ADI has been applied to adults with SCD and vaso-occlusive events (VOE) but has not been investigated in pediatric patients. We explored the role of ADI in pediatric patients with SCD admitted with VOE in order to characterize disadvantage and the hospitalization characteristics that impact hospital readmission.
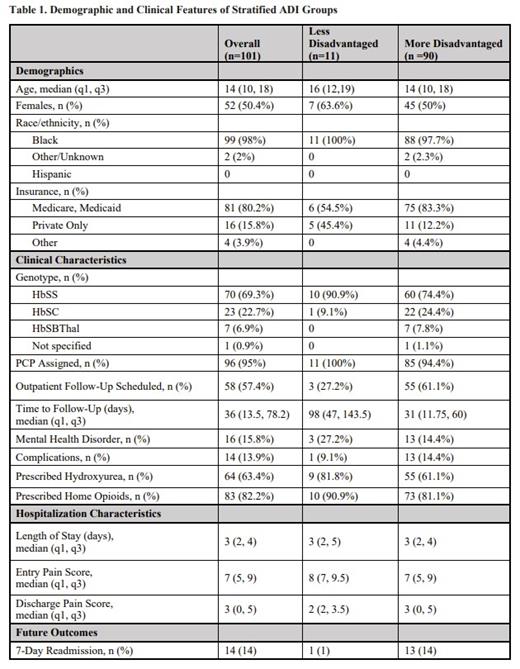
Methods: This retrospective review included 675 consecutive emergency department and hospital admissions for VOE among 101 pediatric (≤ 21 years old) patients with SCD from 2016-2019 at a single urban, US-based medical center. One hospital admission for each patient was selected at random. Information extracted included demographics, SCD characteristics, admission complications, entry and discharge pain scores, length of stay, and management characteristics. Variables were compiled in a descriptive table and compared in logistic regression models against a primary outcome of 7-day readmission.
The 2018 ADI dataset was used to assign an ADI value based on the census block corresponding to the patient-reported zip-code for the specific hospital admission (https://www.neighborhoodatlas.medicine.wisc.edu). ADI values were grouped by most and least deprived with higher scores (6-10) indicating more deprivation. Summary statistics described patient and disease characteristics in these groups.
Results: Within our cohort, the state and national ADI was calculated for 101 patients with a median age of 14 years (50.4% female; 98.0% Black) (Table 1). Most patients were publicly insured (80.2%). The Hb SS genotype was the most common genotype, followed by Hb SC (22.7%). Median ADI rank was 9 with 11 patients (10.9%) classified as less disadvantaged (ADI 1-5) and 90 patients (89.1%) as more disadvantaged (ADI 6-10).
We found the less disadvantaged group had even numbers of public and private insurance use while 83.3% of the patients in the more disadvantaged group had public insurance. The Hb SS genotype was more common in the less disadvantaged (90.9%) than the more disadvantaged (74.4%), where Hb SC was overrepresented (24.4%). Greatest prevalence of mental health disease and hospital complications, including acute chest syndrome, avascular necrosis, and pneumonia, were observed in the more disadvantaged. Additionally, the more disadvantaged group included a greater number of patients with scheduled follow-up (61.1%) and shorter time to follow-up (median: 31 days). For treatment and management, both groups had high numbers of prescriptions for hydroxyurea (HU) and opiates, with slightly higher numbers in the less disadvantaged group (82% HU; 100% opioids) compared to the more disadvantaged (61% HU; 81% opioids). Length of hospital-stay and pain scores were similar across groups. The 7-day readmission rate was 9% for the less disadvantaged group and 14% for the more disadvantaged group.
Conclusions: We applied a validated measure of socioeconomic disadvantage to a group of pediatric patients with SCD and VOE. Our cohort consists of more disadvantaged patients across ADI scales. Readmission rate was low for both groups and there was no relationship between greater ADI scores and hospital readmission. Within the more disadvantaged group, the higher prevalence of mental health illness as well as associated disease complications may have been countered by protective factors including established follow-up, shorter time to follow-up, and high number of prescriptions for hydroxyurea and opiates. Our results are consistent with the protective effect of ADI on recurrent acute chest syndrome in pediatric SCD patients (Alishlash et al. Pediatr. Blood Cancer. 2021) highlighting the importance of preventative care within the SCD medical home. Further research is warranted on identifying key protective factors that may reduce acute care utilization and social disparity in this population.
Novelli: Novartis Pharmaceuticals: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal